I have been thinking a lot about civility in today’s world. There are many days that I feel that it has gone the way of the dodo bird. People close to me have taken long spells of not speaking to me because of my political views. Or more importantly, because my views differ from theirs. Instead of engaging in the conversation, they often become hostile.
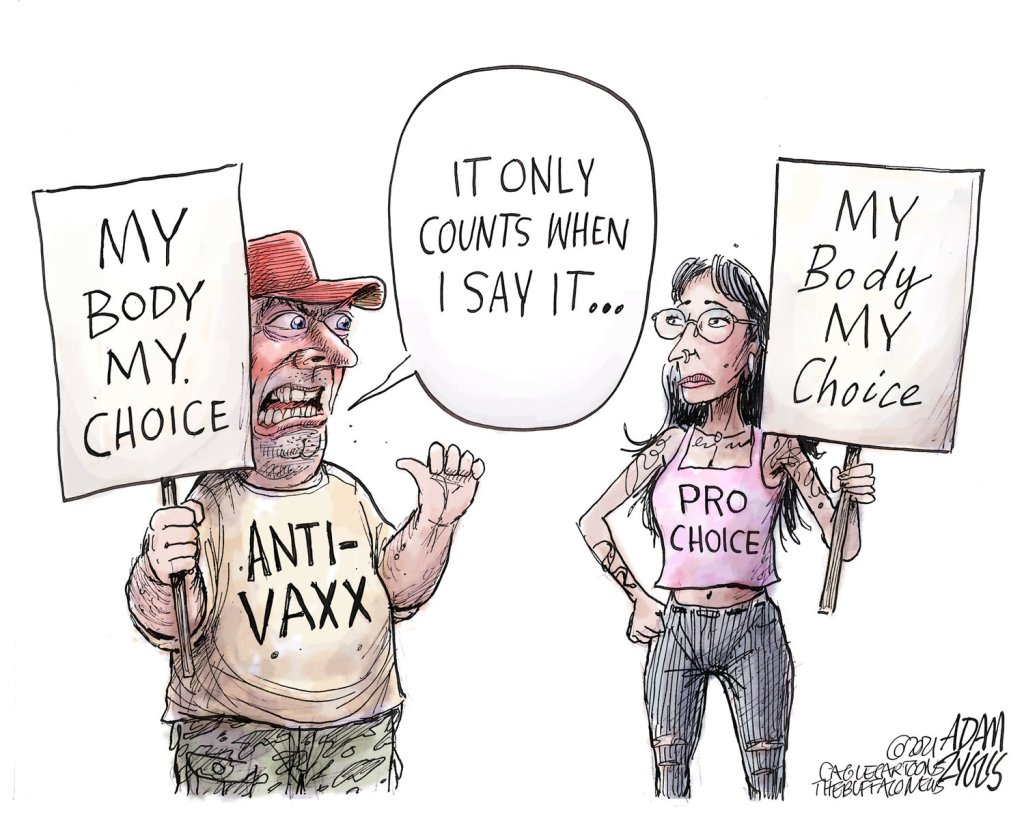
Looking at the political cartoon that I posted, I see an opportunity for people of opposing viewpoints (on completely different topics), to actually come together under a flag of unity.
My husband and I have taken on the idea of teaching our kids how to have a good political discussion. How to disagree without yelling. How to listen without thinking about what you will say next. How to recognize the viewpoint of the other side to show that you are actually listening to what they say.
Not many other people do that. There is one wing of my family that actually walks in lock step with each other politically, and yet you wouldn’t know it based on the loudness of the conversation or how they walk over each other to get the next word in.
At our dinner table, if a fact comes into question during a discussion we will ask them for proof (like here’s your phone, prove it.) In all seriousness, it is because we are teaching our kids to source their material, and to question where they found their fact. Like TikTok is not a reliable resource. And when quoting from a source that is generally regarding as political non-centrist (Fox, MSNBC) that you also find a secondary source. And in that vein, Tucker Carlson is not a news program it is considered political entertainment. By the way, so is Jimmy Kimmel and Stephen Colbert.
I live in a very “red” community. I don’t mind that label. I was born into a conservative family, and raised to love politics. I kept a journal and scrapbook in 1984 on the Reagan vs Mondale election. That was in 5th grade. I LOVED politics.
But today I have to constantly prove myself as a conservative. It’s almost like there is a litmus test and on the surface I don’t pass. Conservatives tell me all of the time that I not a Republican. And since Trump came into office, some of my own family members have called me a RINO (Republican In Name Only).
So let’s go over my political resume . . .
I have been politically obsessed with every presidential campaign since I can remember.
I have a giant scrapbook full of news articles with an accompanied journal for the 84 elections.
Same with the 88 election.
In the 1992 election, I took it one step further and volunteered for the Bush/Quayle election. Joined the College Republicans.
I continued to work on other political campaigns while in college.
While in college, our group decided our campus and newspaper was too liberal, so we decided to start our own underground conservative newspaper called, “The Gipper.”
Then I got married and started having kids.
But I made sure that our kids were raised with both sides being presented. Rush Limbaugh played on the radio as much as NPR.
The older I get, the more my opinions change. I become more settled. My world is more gray and less black and white. My life experiences change who I am. There isn’t anything wrong with that.
I still believe in the big tent theory that Reagan talked about early on in his political career. I see less and less of that with the current leadership of the Republican Party. And frankly I see more of the villian-ization of those who question the totality of the party line. Whey can’t we question? Why can’t we have differing view points?
In the end, I’ve decided that the state of the current political world for conservatives is too toxic. I’m too conservation to be a liberal, and too liberal to be a conservative. I don’t know what it is like to are a part of Democratic Party, so I can only speak to the Republican side. I may not always think in lock step with the party officials, but still believe in the majority of the platform that Republicans endorse.
So back to the political cartoon . . . Wouldn’t it be great if the next frame of this cartoon had both the Anti-vaxxer and the Pro-choice person walking hand in hand towards the sunset while holding a sign that read, “We both support the freedom of choice for our bodies.” or something to that effect.
That would be cool. Even if I disagree or agree with the statement, the fact that both of the protestors acted counter culturally and united when they found commonality between their cause. That be cool. Like really cool . . . like a Jesus kind of cool.